
Fibromyalgia and Integrative Medicine
Fibromyalgia (FM) affects nearly 1 in 20 people globally. In the United States nearly 2–10% of the general population of all ages are affected by this condition. Cost associated with the syndrome exceeds $20 billion. FM is associated with many symptoms: pain, work limitations, low quality of life, poor coping, poor physical functioning. Also multiple chronic co-morbidities can make it particularly challenging to treat. It affects multiple physiological systems: cognitive, musculoskeletal, reproductive, sleep, digestive, urinary and psychological. Evidence-based treatment paradigms are emerging, but there remains a research-to-practice gap, leaving patients to seek out their own treatment options. Patients are increasingly seeking out Traditional Chinese medicine (TCM) for answers concerning FM.
FM BIOMED OVERVIEW
SYMPTOMS
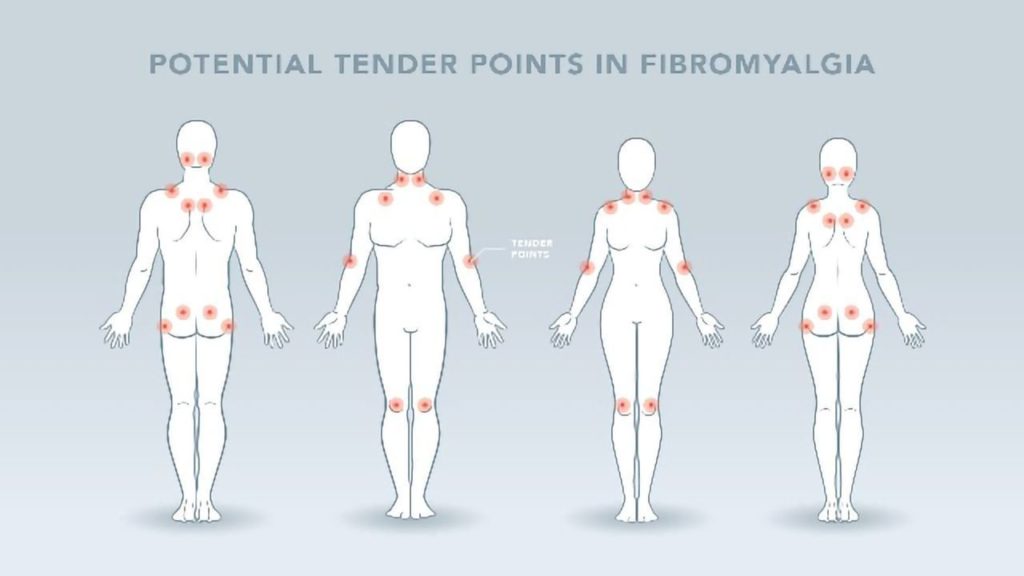
Primarily, FM is a condition characterized by widespread pain, and “tender points” of the muscles and joints on the neck, shoulders, back, hips, arms, and legs. The pain can occur systemically or migrate throughout the body and typically comes and goes over time. FM is most common in women but can also occur in men and usually arises in middle adulthood. FM can be hard to diagnose since there are no lab tests or diagnostics methods to determine if an individual has FM. However, practitioners can suspect fibromyalgia in patients with mostly musculoskeletal pain that is not due to injury or inflammation.
Besides widespread pain and tenderness of the muscles and joints, symptoms of FM also include fatigue, sleep issues, headaches, anxiety, depression, poor memory and problems with thinking or cognitive difficulties. These cognitive difficulties are commonly referred to as “fibro fog” which impairs the ability to focus, pay attention, and concentrate on mental tasks. FM can co-exist with other conditions such as irritable bowel syndrome, migraines, interstitial cystitis, or TMJ.
TYPES OF FM
FM can be either primary (aka idiopathic fibromyalgia), or secondary. In primary FM, the cause is unknown, or the trigger is not present. However, primary FM can be related to an acute stress event such as acute bacterial or viral infections or from a reaction to certain medications. In secondary FM, the cause is clear and is tied to a physical injury or a chronic infectious disease that coexists with the FM condition.
Physical injury can include a neck injury, spinal stenosis, herniated / bulging discs, ankylosing spondylitis, or trauma in the upper spinal region. The chronic infectious diseases include Lyme disease, Hep C or HIV.
Primary FM
It is the more common form of FM. Physical or mental stress from a disease or trauma can trigger microcirculation re-distribution and cause ischemic muscle pain. The peripheral microcirculation reduction due to vasoconstriction triggered by stress acts via the sympathetic nervous system which activates the hypothalamic-pituitary-adrenal (HPA) axis. The HPA axis is the central stress response system. Stress results in cardiovascular dysfunction with vasoconstriction which causes reduced peripheral blood flow in primary FM, although the transient stress is gone, the peripheral vasoconstriction is still persistent.
Secondary FM
Stress and the resulting vasoconstriction are chronic. Overtime, this reduced blood flow leads to the development of ischemic muscle pain. Microcirculation redistribution not only affects the muscles but also the central nervous system in FM patients. Studies have shown a decreased amount of blood flow to the parts of the brain that provide an emotional response to pain and an increased amount of blood flow to the part of the brain that processes pain. This can alter neuron metabolism, brain activity and cause a highly amplified pain sensation to a pain signal as well as cause symptoms of anxiety and depression. Reduced cerebral blood flow is also present with FM patients, causing brain fogginess and affecting cognitive function.
Hyperalgesia / Central Pain Amplification Disorder
In addition to widespread muscle pain from the vasocontraction, FM patients also present with cutaneous hyperalgesia, an increased intensity of pain sensation of the skin. Nociceptive input from deep tissues sensitizes the spinal neurons resulting in the abnormal pain sensation from the skin. This is why FM has been described as a Central Pain Amplification Disorder, meaning the volume of pain sensation in the brain is turned up too high.
ROLE OF NITRIC OXIDE
Nitric Oxide (NO) alteration and oxidative stress is also seen in FM patients.NO is a gasotransmitter and participates in many physiological processes such as vasodilation, modulation of nociception, neurotransmission, and excitation-contraction. Stress induced microcirculation re-distribution can cause decreased levels of NO which further reinforce the microcirculatory disturbances. This may explain why the persistence of vasocontraction after the initial stress factor disappears in primary FM. Oxidative stress due to decreased blood flow can also affect red blood cells (RBCs) since they are susceptible to free radical damage.
RED BLOOD CELLS
A study done at Stanford found that chronic fatigue patients have RBCs that are no longer round and take longer to enter the capillaries and flow through them. Consequently, this may keep them from delivering the correct amount of oxygen to the cells which further aggravate the oxidative stress and cause chronic fatigue symptom. A decreased supply of oxygen to the muscles and cerebrum can affect the amount of ATP produced by the cells mitochondria which can cause tissue acidosis in these areas. High levels of oxidative stress constrict the blood vessels making nutrient delivery deficient. Insufficient amounts of ATP production and other nutrient deficiency in muscles and cerebrum causes not only chronic fatigue but also brain fogginess, sleep issues, headaches, anxiety, depression, poor memory and decreased cognitive function such as math difficulties. There is also a clear connection between FM and the gut biome.
BIOMED TREATMENT
First, chronic pain patients also have a higher rate of ingesting pharmaceutical pain killers at an attempt for temporary symptom relief. Long-term use of pain medication can cause liver damage and liver toxicity. The liver works with the autonomic nervous system. When the liver is weakened it can cause an abnormal neurological repair mechanism which can also result in an abnormal pain response. This may be an additional factor in FM pain and a vicious circle. The Liver is of special interest in TCM.
Eventually, the main modalities for FM treatment in allopathic medicine are: pain meds, anti-depressants and anti-seizure meds, occupational therapy, physical therapy and counseling. I recommend visiting the FM page at Very Well Health for more about Western medicine and FM.

Fibromyalgia & Integrative Medicine
Fortunately, TCM has a more subtle and integrated approach to treating FM.
Above all, in TCM, the main diagnosis for FM are: Liver Qi stagnation, Yin and blood deficiency, Spleen and Kidney yang Deficiency and Kidney Yin deficiency. Using the 5 elements to diagnose can also pave the way for effective treatment plans. Guidance for primary FM includes nurturing Liver and Kidney Yin, activating the Blood and moving Qi. Often associated with NO, Qi is often incorrectly translated as “energy”, a more literal translation would be steam/gas. As far as Qi goes, blockage or stagnation of Qi in the meridians creates pain. Thus, acupuncture usually provides rather fast relief by unblocking Qi. The goal is also to tonify and move the blood with supplements to enhance microcirculation by improving micro-capillary structure and opening up blood circulation.
BLOOD CIRCULATION
By increasing systemic microcirculation, more nutrients and oxygen can get to the muscle tissues and cerebellum for enhanced blood flow. Above all, increased circulation can also help to circulate the free radicals out of the bloodstream and lower the levels of oxidative stress. Patients can experience initial symptom improvement with increased energy levels and mental clarity in one to two weeks. They may experience an increase in the pain initially followed by pain reduction during the first one to two weeks of the protocol. Patients may feel they had the same pain when their condition started: reversal pains after the microcirculation resumes to a normal level. Four to six weeks of a custom botanical formula lead to significant improvement.
For patients with primary FM, the protocol should be able to resolve the condition. However, for secondary FM patients, additional interventions are also required to address the cause(s) of the patient’s FM. For example, if the cause of the FM is due to chronic back pain from a bulging or herniated disc, then we would also include local interventions to contribute to healing the disc injury in order to completely resolve the FM condition. We need to design treatment plans regarding the specific cause of the secondary FM condition.
CONCLUSION
In addition to regular acupuncture and custom formulas we also implement tuina, cupping, guasha and moxibution. Unfortunately, there isn’t “one pill” for treating FM. Consequently, because treating FM requires a multi-pronged approach compliance is paramount. This means taking the formula, doing the exercises, following a sleep schedule, getting acupuncture, etc. In other words, compliance is important for all conditions but PARTICULARLY FOR FM, chronic pain and fatigue. We understand compliance isn’t easy when the results take time; our mission is to support you the patient. We clearly outline a treatment plan and are present for support and follow up.
TCM and Functional Medicine can provide safe, natural, drug free and effective ways to treat FM. Give me a call for a free 15 min consultation to see if I can help you or someone you know with FM and other chronic pain / chronic fatigue issues.
References
- Cao, Huijuan, Jianping Liu, and George T. Lewith. 2010. “Traditional Chinese Medicine for Treatment of Fibromyalgia: A Systematic Review of Randomized Controlled Trials.” Journal of Alternative and Complementary Medicine 16 (4): 397–409.
- Dellwo, Adrienne. n.d. “The Big List of Fibromyalgia Symptoms.” Accessed October 14, 2021. https://www.verywellhealth.com/fibromyalgia-symptoms-716139.
- “Fibromyalgia.” n.d. Accessed October 14, 2021. https://www.mayoclinic.org/diseases-conditions/fibromyalgia/diagnosis-treatment/drc-20354785.
- Li Chang-Du, Fu Xiao-Ying, Jiang Zhen-Ya, Yang Xu-Guang, Huang Si-Qin, Wang Qiong-Fen, Liu Jia, and Chen Yuan. 2006. “[Clinical study on combination of acupuncture, cupping and medicine for treatment of fibromyalgia syndrome].” Zhongguo zhen jiu = Chinese acupuncture & moxibustion 26 (1): 8–10.
- Mist, Scott D., Cheryl L. Wright, Kim Dupree Jones, and James W. Carson. 2011. “Traditional Chinese Medicine Diagnoses in a Sample of Women with Fibromyalgia.” Acupuncture in Medicine: Journal of the British Medical Acupuncture Society 29 (4): 266–69.
- Mist, Scott, Cheryl Wright, Kim D. Jones, James W. Carson, and Jean Shih. 2010. “Traditional Chinese Medicine for Fibromyalgia.” Practical Pain Management 10 (7). https://www.ncbi.nlm.nih.gov/pubmed/25383059.
- Schweiger, Vittorio, eta al 2020. “Comparison between Acupuncture and Nutraceutical Treatment with Migratens® in Patients with Fibromyalgia Syndrome: A Prospective Randomized Clinical Trial.” Nutrients 12 (3). https://doi.org/10.3390/nu12030821.
- Yuan, Qi-Ling, et al. 2016. “Acupuncture for Musculoskeletal Pain: A Meta-Analysis and Meta-Regression of Sham-Controlled Randomized Clinical Trials.” Scientific Reports 6 (July): 30675.

